menu

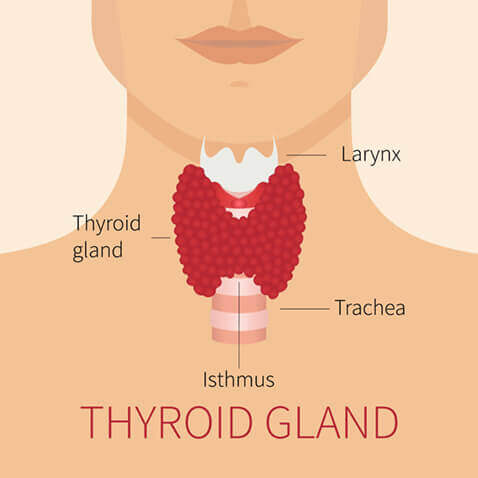
The thyroid gland is a butterfly-shaped gland located in the low anterior neck. It produces thyroid hormone, which helps to regulate the body’s metabolism. The functional capacity of the thyroid is measured by blood tests. Excessive production of thyroid hormone (hyperthyroidism) can cause palpitations, tremors, weight loss, and heat intolerance. Conversely, an under-active thyroid gland (hypothyroidism) can result in fatigue, weight gain, and cold intolerance.
A thyroid nodule is a growth in the thyroid gland. Thyroid nodules are extremely common, and may be solitary or multiple (multinodular goiter). It is estimated that approximately 5-10% of the population has a palpable thyroid nodule, and between 30-85% have tiny thyroid nodules that are too small to palpate.
In most people with thyroid nodules, the gland produces a normal level of thyroid hormone (euthyroid state). Statistically, approximately 5-10% of nodules are cancerous. Some patients have findings that increase the risk of malignancy. A history of exposure to radiation to the neck is such a risk factor, as is a family history of thyroid cancer. Hoarseness, lymph node enlargement, and fixation of the nodule can also increase the risk of malignancy. Fortunately, the vast majority of thyroid cancers are treatable and carry an excellent prognosis.
Most thyroid nodules do not require surgery. The primary indications for thyroidectomy are suspicion of cancer, large size, substernal location (nodules that grow inferiorly into the chest), or symptoms (throat pressure, difficulty swallowing, respiratory distress, or cosmetic disfigurement from a visible goiter). Over-functioning nodules are sometimes best treated by surgery, as well.
The most important tests to evaluate a thyroid nodule are Ultrasound of your thyroid (shows size, location and characteristics of the nodule), a TSH level (a blood test that evaluates the function of the gland) and a fine needle aspiration (FNA) biopsy to evaluate the nodule for malignancy. Although FNA is highly accurate, it is not 100% accurate in making a diagnosis. FNA is usually performed by Radiologists under ultrasound guidance. There are some types of thyroid nodules (follicular tumors) where FNA cannot distinguish benign from malignant nodules- these nodules are usually best managed by thyroidectomy.
Thyroid operations can be divided into several categories, including a unilateral lobectomy (“one-sided” removal of the thyroid gland), total thyroidectomy (removal of both sides of the thyroid gland), or variations in which all of one side of the gland and part of the other side of the gland are removed.
Thyroid surgery is an operation to remove part or all of the thyroid gland. It is performed in the hospital under general anesthesia. Typically the operation removes the lobe of the thyroid gland containing the lump for diagnosis, or possibly the entire gland if you have a large goiter or have been diagnosed with a thyroid carcinoma. A frozen section (an immediate microscopic reading) may or may not be used to determine if the rest of the thyroid gland should be removed. If you have specific questions about thyroid surgery, ask your otolaryngologist and he or she will answer them in detail.
Patients who have a unilateral (one-sided) thyroidectomy will usually spend one night in the hospital, have their drain removed on the morning after their surgery. If you go home with a drain you will be taught by the nurses how to change your dressing. You will see a semicircular or curved incision just above the breastbone, which will be your thyroidectomy surgical incision site.
Patients having a total or subtotal thyroidectomy (operation on both sides of the gland) will usually spend one to two nights in the hospital in order that their calcium levels are monitored closely, as low calcium levels are a complication seen only with the more comprehensive removal of thyroid tissue. Total and subtotal thyroidectomy patients will usually also have a drain in the neck. You will usually have your drain removed the day after surgery before you leave the hospital. Unless instructed otherwise by your surgeon, the incision may be left open to the air.
Patients will usually be given a prescription for pain medicine, which is to be used as needed. In some cases, you will be also sent home with either a new or continuing prescription for Synthroid, levothyroxine, or Cytomel (thyroid replacement or suppression medication) and this must be used on a regular daily basis at the dose prescribed by your doctor. Calcium and Vitamin D supplements are sometimes prescribed as well.
Many patients notice a subtle change in their voice quality for the first few weeks postoperatively. Although trauma to the nerves supplying the vocal cords on one or both sides of the voice box may occur during thyroidectomy, frank hoarseness or trouble swallowing is a very rare complication. If you have any questions regarding the fact that your voice may be excessively hoarse or raspy, or if you are experiencing any type of coughing or choking when you attempt to swallow, please call our office immediately.
For patients undergoing a total or subtotal thyroidectomy, normal calcium levels the first several days while hospitalized do not always predict stable blood calcium levels. Occasionally, patients have significant dips in their blood calcium levels after their discharge from the hospital due to manipulating or “bruising” of the parathyroid glands. The symptoms of low calcium would include tingling around the mouth or in the hands or feet, generalized weakness, or feelings of the heart exhibiting an abnormal rate or irregular beat. If any of these symptoms occur, please call our office immediately.
A potentially serious or life-threatening complication of thyroidectomy, which can occur rather abruptly, is formation of a hematoma from a bleeding blood vessel or other area deep in the neck tissues. If you would at any point feel that there has been an abrupt swelling or outward displacement of the wound area in the lower neck, or if the neck wound suddenly starts exhibiting more tenderness, redness, or bogginess than you would expect, you need to contact our office immediately. If any shortness of breath would begin to develop, you are directed to proceed to the emergency room at the hospital where your surgery was performed as quickly as possible.
Please refer to After Thyroid Surgery for post-operative instructions.